
Colonoscopy
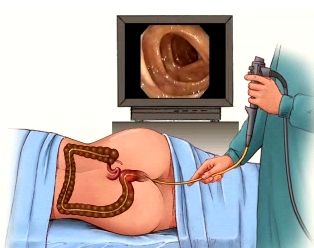
Colonoscopy is a test which allows the doctor to look directly at the lining of the large intestine (the colon). Diagnostic colonoscopy is recommended for alterations in bowel habits, occult or frank blood in the stool, unexplained anaemia and as a screening test for colon cancer. In order to do the test a colonoscope is carefully passed through the anus into the large intestine. The colonoscope is a long flexible tube, about the thickness of your index finger, with a bright light at its tip. The video camera on the colonoscope transmits images of the inside of the colon to a monitor allowing the physician to examine the lining of the colon checking for any disease or abnormalities.
The physician may take a biopsy - a sample of the lining of the bowel for closer examination under the microscope. A small piece of tissue is removed painlessly through the colonoscope, using tiny biopsy forceps.
It is also possible to remove adenomas (polyps) during colonoscopy. Polyps are abnormal projections of tissue, rather like a wart, which the doctor will want to remove and examine in more detail.
Preparation
To allow a clear view, the colon must be completely empty of waste material. If it is not, certain areas may be obscured and the test may have to be repeated. The links below provide information on patient preparation for a colonoscopy procedure.
Bowel preparation instructions for colonoscopy am & pm appointments
Bowel preparation instructions for colonoscopy when carried out with an upper endoscopy (OGD)
- morning appointments
Bowel preparation instructions for colonoscopy when carried out with an upper endoscopy (OGD)
- afternoon appointments
Diabetic colonoscopy patient advice (insulin or tablet controlled)
Diabetic colonoscopy patient (insulin or tablet controlled) example light diet
It is important to take all of the laxative prescribed and also considerably increase your intake of clear fluids on the day before the examination, which will help clean the bowel.
When you come to the department, a member of staff will explain the test to you and will usually ask you to sign a consent form. This is to ensure that you understand the test and its implications. Please tell the doctor of nurse if you have had any allergies or bad reactions to drugs of other tests. They will also want to know about any previous endoscopy you have had, or of any other medical conditions which you may suffer from and any medication which you may be taking. If you have any worries or questions at this stage don't be afraid to ask. The staff will want you to be relaxed as possible for the test and will not mind answering your queries.
What will happen?
You will be placed in a comfortable position on your left side, and may be given medication by injection through a vein to make you sleepy and relaxed. The doctor will then pass the colonoscope through the anus into the rectum, and advance it through the colon. You may experience some abdominal cramping and pressure from the air which is introduced into your colon. This is normal, and will pass quickly. You may also be asked to change position during the examination, and will be assisted by a nurse. The examination takes 15-60 minutes.
Afterwards
You will be left to rest in the recovery area for up to 1 hour, until the main effects of any medication wear off. A responsible adult must be available to escort you home as the sedation impairs your reflexes and judgment. For the remainder of the day you should not drive a vehicle, operate machinery or make important decisions. We suggest that you rest quietly.
When will I know the results?
In many cases the doctor will be able to tell you the results of the test as soon as you are awake. However if a biopsy sample or polyp was removed for closer examination, these results may take up to ten days to process.
Many patients find that sedation tends to make them forget any explanations that may have been given them. Details of any results or further investigations may be obtained from your GP or specialist (whoever referred you for the test).